Without trying to sound completely reductionist – us women are a bunch of ever changing hormones. We don’t know where we are from one week to the next! With a regular menstrual cycle orchestrated by differing levels of oestrogen, progesterone, follicle-stimulating hormone and luteinising hormone black blah blah (I appreciate that I’ve wacked in some big names there – I will describe these hormones to you further on) our bodies and moods are thrown all over the shop.
Something that really does my swede in is our acceptance of feeling like shit, but not actually knowing why we feel this way. This is especially true during the perils of growing and popping out a baby – a whole world away from the regular cycle we may have been in tune with previously.
I’m not going to lie, this post is more of a human biology lesson, but details the hormonal changes you go through before and after childbirth and some of the symptoms that may play havoc with your body. I hope this helps mums understand a little more just how complex we all are…

What is a ‘regular’ menstrual cycle?
So let’s talk about your period, menzies, time of the month or in our house, we call it ‘blobby blobs’ – this will help us understand just how messed up our hormones can get during our menstrual cycle. For the purpose of this, we will go textbook generic cycle talk…
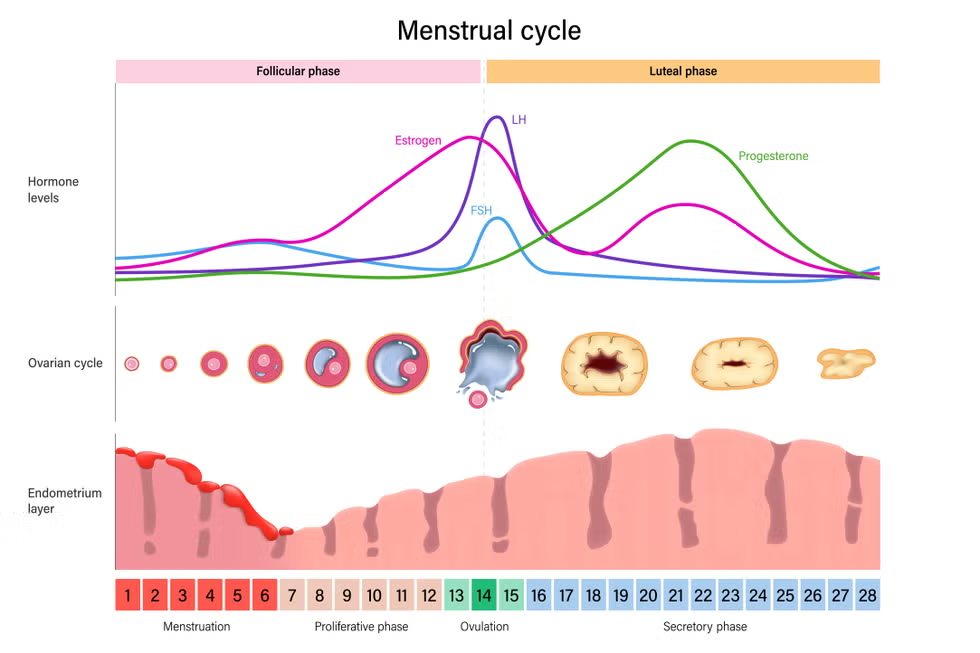
A regular menstrual cycle typically lasts about 28 days, but it can range from 21 to 35 days. The cycle is controlled by a balance of hormones, mainly oestrogen and progesterone, which prepare the body for pregnancy each month. It starts with the menstrual phase, when bleeding occurs, marking the beginning of the cycle. This phase usually lasts 3 to 7 days. During this time, oestrogen levels are low, and the lining of the uterus (endometrium) is shed because there’s no pregnancy.
As the cycle progresses, oestrogen levels rise, helping to thicken the uterine lining in preparation for a possible pregnancy. Around the middle of the cycle, usually day 14, ovulation occurs — this is when an egg is released from the ovary. After ovulation, progesterone levels increase to help maintain the uterine lining, making it ready for a fertilised egg. If the egg isn’t fertilised, progesterone and oestrogen levels drop, triggering the start of a new cycle with menstruation.
Common symptoms throughout the cycle can include mood swings, bloating, breast tenderness, and cramps, especially just before or during menstruation.
Here’s a pretty picture to sum that all up…
So this is ‘normal’ but what do our hormones look like after having a baby? How do hormones hugely impact a women’s ability to ‘bounce’ back to normal, not only after having a baby but when transitioning from mother-to-be to new mother and the journey of your body readjusting itself throughout the postpartum journey.
Even if you are able to take 9 – 12 months off work after having a baby, did you know that at 9 months postpartum your body is still in recovery? Your hormones are still very much not ‘bouncing back’ just like you are supposed to. So what does that look like? You may still be breastfeeding at this stage, you might not – there are so many factors which contribute to how your body recovers hormonally after having a child. Let’s talk about how that might look and feel…
Hormonal changes during pregnancy

Let’s break down how the female body hormones change during pregnancy, so you can have a little more confidence that you aren’t or weren’t going insane…
Oestrogren and progresterone
These hormones rise steadily throughout pregnancy, supporting the development of the foetus and preparing the body for childbirth. Elevated levels can influence mood and physical wellbeing. Personally, during my second pregnancy I was an absolute witch, moody as hell, grumpy as sin and in both pregnancies I got these strange little skin tags all over my neck and back. Thanks hormones!
During pregnancy, oestrogen and progesterone cause various physical and emotional symptoms. Oestrogen contributes to nausea, breast enlargement, increased skin pigmentation (melasma), mood swings, nasal congestion, and increased vaginal discharge, as well as fluid retention and swelling.
Progesterone, which is essential for maintaining pregnancy, can lead to fatigue, bloating, constipation, dizziness, low blood pressure, increased body temperature, and pelvic discomfort due to its muscle-relaxing effects.
Both hormones play a role in breast tenderness, mood changes, and overall pregnancy-related discomfort, with oestrogen more linked to nausea and skin changes, and progesterone is more associated with bloating, digestion issues, and muscle relaxation.
Human chorionic gonadotropin (hCG)
This is produced by the placenta, maintaining something called the corpus luteum (sounds a bit Harry Potter if you ask me) which ensures that progesterone is continuously produced during early pregnancy so we can keep that uterus lining nice and thick, rather than shedding like you would during your regular menstrual cycle.
hCG causes various physical and emotional changes during early pregnancy. Common symptoms include nausea and vomiting (morning sickness), fatigue, breast tenderness, frequent urination, bloating, and digestive issues.
Many women also experience mood swings, heightened emotions, anxiety, or irritability due to hormonal fluctuations. Skin changes, such as increased oil production, acne, or darkening, can also occur. Higher hCG levels are often linked to more severe morning sickness, while low or slow-rising levels may indicate pregnancy complications.
Oxytocin
This is otherwise known as the love hormone, it’s levels increasing towards the end of pregnancy, promoting uterine contractions during labour and enhancing bonding between mother and baby
Oxytocin, often called the “love hormone,” increases towards the end of pregnancy and plays a crucial role in labour, birth, and bonding. Rising oxytocin levels trigger uterine contractions, helping to progress labour and eventually deliver the baby. During and after birth, it promotes mother-infant bonding by enhancing feelings of love, trust, and emotional connection. Oxytocin also stimulates the let-down reflex for breastfeeding, allowing milk to flow more easily. Some women may experience strong contractions, afterbirth pains, or heightened emotions due to oxytocin surges. Additionally, it contributes to a sense of calm and well-being, reducing stress and promoting relaxation after childbirth.

Afterbirth pains
Although this is a postpartum snippet of information, let’s talk a bit more about those ‘afterbirth pains.’ This happened to me after both births but the first time I didn’t expect it and the pain was excruciating – I genuniely thought I’d have to ring 999.
Although pre-baby classes are super helpful for genning us up on all the info needed about birth, I felt like someone failed to tell me this. Maybe I just got them so much worse than some other women do, but I tell you it was like labour again!
Afterbirth pains, also known as postpartum uterine contractions, occur as the uterus contracts back to its pre-pregnancy size after childbirth. These pains are a normal part of the recovery process and are most noticeable in the first few days following delivery. The hormone oxytocin plays a key role in triggering these contractions, as it helps the uterus shrink and get rid of any remaining placenta tissue. Breastfeeding also stimulates oxytocin release, which can make the contractions more intense, particularly during the early postpartum period.
The discomfort from afterbirth pains is often compared to strong menstrual cramps and can last for a few days to a week, gradually reducing in intensity. Women who have had multiple births may experience stronger pains as the uterus requires more effort to return to its normal size. Pain relief, along with warm compresses, can help alleviate the discomfort. While these pains are typically temporary and part of the body’s natural healing, persistent or severe pain should be discussed with a healthcare provider to ensure there are no complications.
Anyway – back to pregnancy hormones…
Prolactin
Prolactin is a hormone that prepares the breasts for lactation, with levels rising throughout pregnancy to support milk production after childbirth. As prolactin increases, it can cause breast enlargement and tenderness, as the mammary glands develop in preparation for breastfeeding. Many women may also experience increased sensitivity in the breasts or a feeling of fullness as the body readies itself for milk production. After birth, prolactin helps stimulate milk production when breastfeeding, leading to leaking breasts or colostrum (early milk) production in the first few days. In some cases, mood changes, including feelings of calm or relaxation, may also occur as prolactin works in conjunction with other hormones to facilitate breastfeeding. Additionally, high levels of prolactin can sometimes lead to irregular periods or even temporary cessation of menstruation while breastfeeding.

Let’s talk about postpartum hormones…
Oestrogen and Progesterone
After childbirth, levels of oestrogen and progesterone drop quickly, which can contribute to the emotional changes many women experience, including mood swings or the “baby blues”. This hormonal shift often leads to feelings of tearfulness, irritability, or overwhelm, and is common in the first few days to weeks after delivery. For non-breastfeeding mothers, oestrogen and progesterone levels tend to return to pre-pregnancy levels more quickly, which may lead to their period’s resuming sooner compared to breastfeeding mothers. However, this rapid hormonal change can also cause vaginal dryness and mood fluctuations, as the body adjusts.
Oxytocin
Levels of oxytocin remain high immediately after birth, playing a crucial role in uterine contractions that help reduce postpartum bleeding and return the uterus to its pre-pregnancy size (see above for afterbirth pains). It also promotes emotional bonding between mother and baby by fostering feelings of affection and attachment. While breastfeeding mothers experience oxytocin surges during nursing, non-breastfeeding mothers still benefit from these bonding effects, though they may not experience the same intensity of the let-down reflex that stimulates milk production.
Prolactin
For both breastfeeding and non-breastfeeding mothers, prolactin levels increase postpartum. In breastfeeding mothers, prolactin is essential for milk production. However, for those who do not breastfeed, prolactin levels will still rise initially but will decrease quickly after birth. This drop means that non-breastfeeding mothers will not experience the same level of breast fullness or leaking that breastfeeding mothers do. However, they may still experience breast tenderness or a feeling of engorgement as the body adjusts to the lack of milk production.
Hormonal Changes in the weeks and months postpartum
Oestrogen and Progesterone
In the weeks and months following childbirth, oestrogen and progesterone gradually return to their pre-pregnancy levels. For non-breastfeeding mothers, this typically happens more quickly than for breastfeeding mothers. The return of oestrogen often signals the menstrual cycle to fire back up again, sometimes as early as 6 to 8 weeks postpartum. The return of progesterone helps regulate the reproductive system, although it can also lead to irregular periods in the early months. Some women may experience vaginal dryness and decreased libido as oestrogen levels stabilise.
Prolactin
For non-breastfeeding mothers, prolactin levels gradually return to normal postpartum. Without the regular stimulation of breastfeeding, prolactin levels drop, stopping any milk production. This can cause some discomfort, such as breast engorgement, but typically, the body will adjust and milk production will cease after a few days to weeks. If breastfeeding, mothers will experience fluctuations in prolactin, and they may feel breast tenderness or leakage as time passes.
Cortisol
Cortisol, the “stress hormone,” can be elevated postpartum, particularly due to the physical and emotional demands of caring for a newborn. For both breastfeeding and non-breastfeeding mothers, elevated cortisol levels can cause feelings of irritability, anxiety, or fatigue, especially when sleep deprivation and the adjustment to a new routine take a toll. Elevated cortisol can also impact immune function and energy levels, making it important for mothers to find ways to manage stress and prioritise rest and self-care.
Long-term hormonal changes
Over time, hormonal changes continue to shape a woman’s body and emotions as she adjusts to life after childbirth. For non-breastfeeding mothers, oestrogen and progesterone levels will stabilise relatively quickly, with menstrual cycles returning within a few months. For breastfeeding mothers, these hormones may remain low for longer to support lactation. In both cases, prolactin levels will return to normal as breastfeeding decreases or stops, leading to the cessation of milk production. Cortisol levels may remain elevated for some time as new mothers continue to adjust to the demands of caring for their baby (toddler, child, teenager…does it stop?!), with stress management being essential for overall well-being.
For all mothers, adjusting to these long-term hormonal changes can also affect mental health. Hormonal fluctuations may contribute to postpartum depression or anxiety, particularly as women navigate the physical and emotional challenges of early motherhood. Understanding these changes and seeking support when needed is crucial for maintaining health during the postpartum period.
After childbirth, hormonal changes are a natural and crucial part of the recovery process, helping the body heal and adjust to life as a mother. However detailed I have gone with symptoms of your changing body, each and every woman’s hormonal journeys will differ, we aren’t textbook and sometimes things just don’t go how they are supposed to. I spent months freaking out about how I physically felt my hormones were not ok, however because I had ultimately passed that postpartum sweetspot where my hormones should be fine and dandy, I just could not figure why I felt this way – putting it down to ‘this is just me now’ although I completely felt not who I should be.
Sometimes we don’t resolve…
Hey, strangely enough in some cases, hormonal imbalances or dysfunctions can occur, causing longer term symptoms and leading to a range of issues that may impact a mother’s physical and emotional well-being. These issues can arise from irregular hormonal fluctuations or conditions that affect hormone production, potentially causing symptoms that disrupt daily life. Below is a list of potential complications that may occur when hormones do not behave in the typical way after childbirth:

Postpartum thyroiditis
Inflammation of the thyroid gland after childbirth, leading to symptoms like fatigue, weight changes, mood swings, and irregular periods. It can cause periods of hyperthyroidism (high thyroid levels) followed by hypothyroidism (low thyroid levels).
Persistent low libido
Low levels of oestrogen and testosterone after childbirth can lead to persistent low libido or a lack of sexual desire. This may be compounded by vaginal dryness or discomfort during sex.
Postpartum depression (PPD)
A severe form of mood instability, anxiety, and sadness that can persist beyond the baby blues due to hormonal fluctuations, particularly oestrogen, progesterone, and cortisol levels.
Prolactin imbalance
Excessive prolactin can lead to breast engorgement, leaking, or lactation failure, while insufficient prolactin may cause issues with milk supply or inability to breastfeed.
Hormonal imbalance in menstrual cycles
Irregular periods or amenorrhea (absence of menstruation) can occur, especially if breastfeeding, as oestrogen and progesterone levels are suppressed for longer periods.
Pelvic organ prolapse
After childbirth, particularly after vaginal delivery, hormonal changes can weaken the pelvic floor muscles, leading to pelvic organ prolapse, where the bladder, uterus, or rectum may descend into the vaginal canal.
Osteoporosis
Low levels of oestrogen (especially during prolonged breastfeeding) can lead to bone density loss, increasing the risk of fractures and osteoporosis.
Vaginal dryness and pain
Lower oestrogen levels postpartum can lead to vaginal dryness, pain during intercourse, and vulvar irritation, which can affect sexual health and comfort.
Cortisol imbalance and anxiety
Elevated cortisol levels due to chronic stress or sleep deprivation can result in prolonged feelings of anxiety, fatigue, and irritability, impacting mental health.
Adrenal fatigue
Chronic stress postpartum can lead to adrenal fatigue, where the adrenal glands (which produce cortisol) are overworked, causing chronic tiredness, difficulty coping with stress, and feelings of being overwhelmed.
These conditions, though less common, can significantly impact postpartum recovery and well-being. It’s important for new mothers to seek medical advice if they experience prolonged or unusual symptoms, as addressing hormonal imbalances early can help ensure better overall health and recovery.
So you aren’t going mad after all…
So, if you’ve ever felt like your body’s been hijacked by a chaotic cocktail of hormones — you’re not alone, and you’re definitely not imagining it.
From the regular ups and downs of your menstrual cycle to the total hormonal upheaval of pregnancy and postpartum life, our bodies go through a lot. And while we often just accept feeling off, moody, or downright broken, understanding the science behind it all can be empowering (and a little comforting, too). There are natural methods which may alleviate your symptoms which are definitely worth exploring, before you commit to the hard stuff and is something I support my ladies with.
Motherhood isn’t just nappies and sleepless nights — it’s a full-body, hormone-fuelled transformation that deserves way more recognition, support, and honesty. So next time you’re feeling out of sorts, remember: it might just be your hormones — and they’ve got one hell of a story to tell.

Some definitions from above (because we ain’t all science nerds)
Follicular development: Follicular development is the process where tiny sacs in the ovaries, called follicles, grow and prepare to release an egg. Each month, one follicle matures, and when it’s ready, it bursts open to release an egg for possible fertilisation. This process is controlled by hormones and is a key part of the menstrual cycle.Follicular development: Follicular development is the process where tiny sacs in the ovaries, called follicles, grow and prepare to release an egg. Each month, one follicle matures, and when it’s ready, it bursts open to release an egg for possible fertilisation. This process is controlled by hormones and is a key part of the menstrual cycle.
Ovulation: Ovulation is when a mature egg is released from the ovary. This happens about halfway through the menstrual cycle and is the best time for pregnancy to occur if sperm is present.
Uterus: The uterus is a hollow, muscular organ in a woman’s body where a baby grows during pregnancy. It’s also where the lining builds up each month and sheds during a period if there’s no pregnancy or that we need to keep nice and thick when pregnant.

Leave a comment